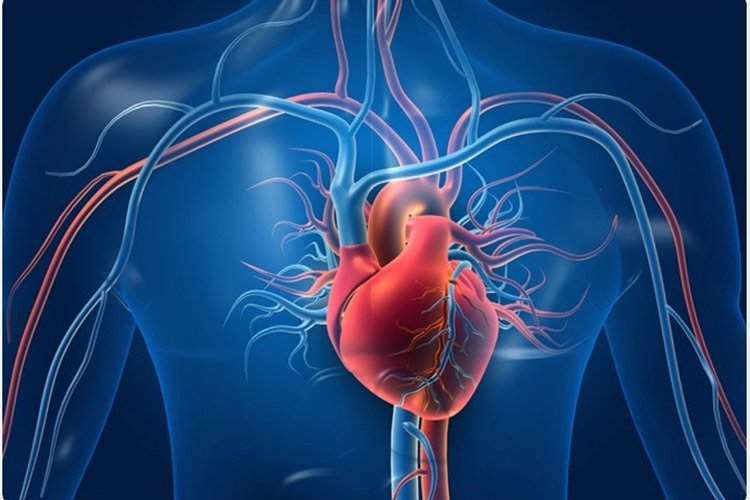
Blood circulation is vital to our health. Our arteries carry oxygen, energy-rich nutrients, hormones, immune cells and other essentials throughout the body. If the supply is interrupted, organs and tissues can be irreversibly damaged within minutes.
But a second part of blood circulation is also vital: the return journey. After our arteries deliver the goods, our blood must return to the lungs to pick up more oxygen, absorb nutrients, get rid of carbon dioxide and flow back to the heart to be pumped out again. This way, the blood is in constant motion, ensuring that organs and tissues get what they need while waste products are removed.
The vessels designed to make the return journey are your veins. Read on to get answers to questions about how veins work, what can affect their smooth functioning and five ways to keep thousands of miles of these blood vessels healthy.
Maybe you haven’t given your veins much thought. Or if you have, you may have focused on varicose veins, those swollen, unsightly purple vessels that can be visible just under the skin of the legs. Or maybe you’ve had a blood test and the person who drew the blood had trouble finding a “good vein.” But that’s just a small part of the world of veins.
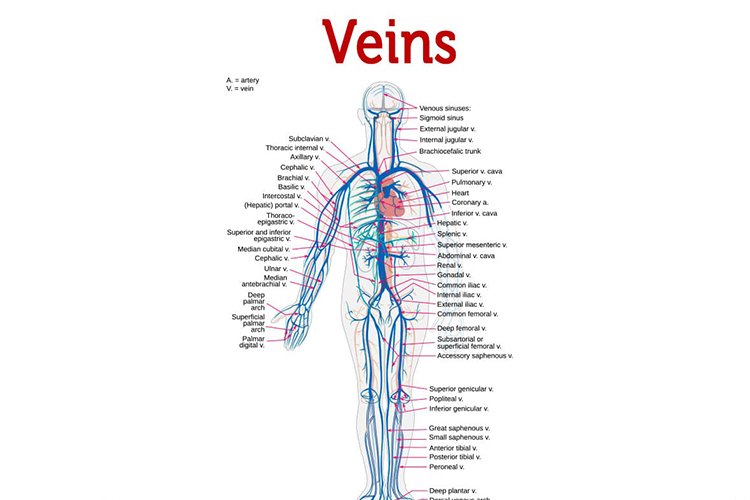
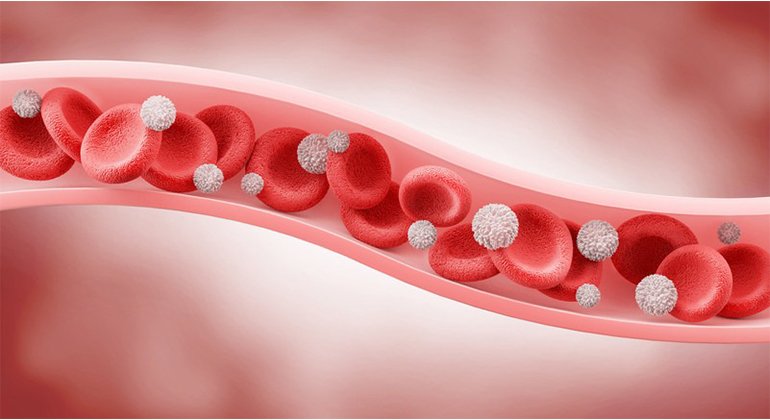
Veins form a network of connecting tubes throughout the human body, ranging in size from 1 mm (about the size of a pencil tip) to 2 cm (about the size of a quarter), that bring deoxygenated blood back to the lungs to recharge with oxygen. Then four pulmonary veins carry oxygenated blood from the lungs to the heart. (Fun fact: Some people have three or five pulmonary veins, but most of us have four.)
Often, large veins are found next to similarly named arteries, like on a highway with cars traveling in opposite directions: In the upper arm, for example, the axillary vein lies next to the axillary artery; in the kidney, the renal vein runs next to the renal artery.
First, let’s imagine tiny red blood cells loaded with oxygen. Now imagine you’re a red blood cell that just traveled from the heart through the arteries to a jogger’s calf muscle. After delivering much-needed oxygen and taking in waste products like carbon dioxide, you need to get back to the heart quickly because muscles need extra oxygen when exercising.
But wait. The journey back to the lungs to take in more oxygen and release carbon dioxide is a steep uphill climb. How can you make it back to the lungs without help?
Fortunately, veins have tiny valves that allow blood to flow in only one direction. When muscles near larger veins contract, they pump blood toward the lungs. Additionally, inhaling creates a sort of suction that pulls blood toward the lungs. Without these forces encouraging blood to flow through the veins in the right direction, blood flowing into the legs would pool there, causing dangerously high pressure and swelling.
In fact, they’re not. People think they’re blue because that’s how they often appear in diagrams and illustrations. But that’s just to distinguish them from the bright red arteries.
The veins on the back of your hand may appear blue if you have fair skin. That’s an illusion caused by the way light is absorbed by the skin. In people with darker skin tones, the veins tend to blend together more.
If you could look at veins directly without skin in the way, they would appear pale because they are naturally colorless, or dark red because of the blood in them.
Blood clots, varicose veins, and venous insufficiency are some of the most common health conditions that affect the veins:
Deep vein thrombosis (DVT) occurs when a blood clot forms in a deep vein, blocking blood flow. This condition is potentially serious because clots in deep veins can travel to the lungs and cause a life-threatening pulmonary embolism by blocking an artery that carries blood to part of the lungs.
Superficial thrombophlebitis is a blood clot in a small vein just under the skin. This causes inflammation and pain.
Varicose veins are small veins under the skin that swell and twist. While these can be harmless, they can cause pain and are occasionally complicated by blood clots.
Venous insufficiency occurs when the valves of the veins are damaged – for example, due to aging or previous blood clots. Blood flow through veins can be compromised, causing leg swelling, increased pressure, inflamed skin and poor healing.
A far rarer condition has the evocative name of phlegmasia cerulea dolens. It is a serious complication of deep vein thrombosis in which obstruction of blood flow through a deep vein leads to blockage of blood flow through nearby arteries. This can lead to gangrene and amputation.
All of these conditions can temporarily or permanently impair circulation. Treatments aim to restore circulation where possible.
Healthy veins help the heart, brain and every other part of your body. Here are five ways to improve vein health, even if you already have vein disease:
Be active. Exercise regularly and avoid standing or sitting for long periods of time.
Choose healthy foods, such as those from a plant-based, heart-healthy diet.
Maintain a healthy weight.
Don’t smoke.
Wear compression stockings if you already have a vein condition such as venous insufficiency.
And of course, if you experience unexplained swelling, inflammation or ulcers on your legs, ankles or feet, you should see a doctor.
The bottom line: Our veins are busy 24/7 carrying blood from far away places back to the lungs and heart, which pumps enriched blood out again. Without veins, blood circulation would not be possible. They are a good example of how many parts of your amazing body are easily overlooked until something goes wrong.